I watch, listen to and read a significant amount of health-related information. Some of it is to be certified professionally in an area, some of it is to better help myself and my clients, and some of it is just interesting to me. There is a topic that seems to be everywhere lately, (if you’re in to the subject of natural health and nutrition), and that is the importance of the ‘microbiome’.
You literally have an entire world of creatures living inside and on you. Your body is full of trillions of bacteria, viruses, parasites and fungi, that coexist in your GI tract, nose and skin, among other places. Collectively these organisms are known as the microbiome, and they may outnumber human cells by many trillions.
Science is continually realizing how important the microbiome is to various aspects of human health. Much of the time these organisms are beneficial to human health, but sometimes, they can cause harm. And sometimes, the organisms are helpful in certain amounts, and harmful if over that threshold.
These organisms get to live with us as their hosts, and in payback, their jobs are to help us digest food, protect against pathogens that want to move in; help synthesize vitamins, enzymes and hormones, protect against inflammation, help our immune system function, help with metabolism and help with mood and cognition. That is asking a lot, and so, our microbiota ask that, in return, we nourish them properly, so that they can continue their important work.
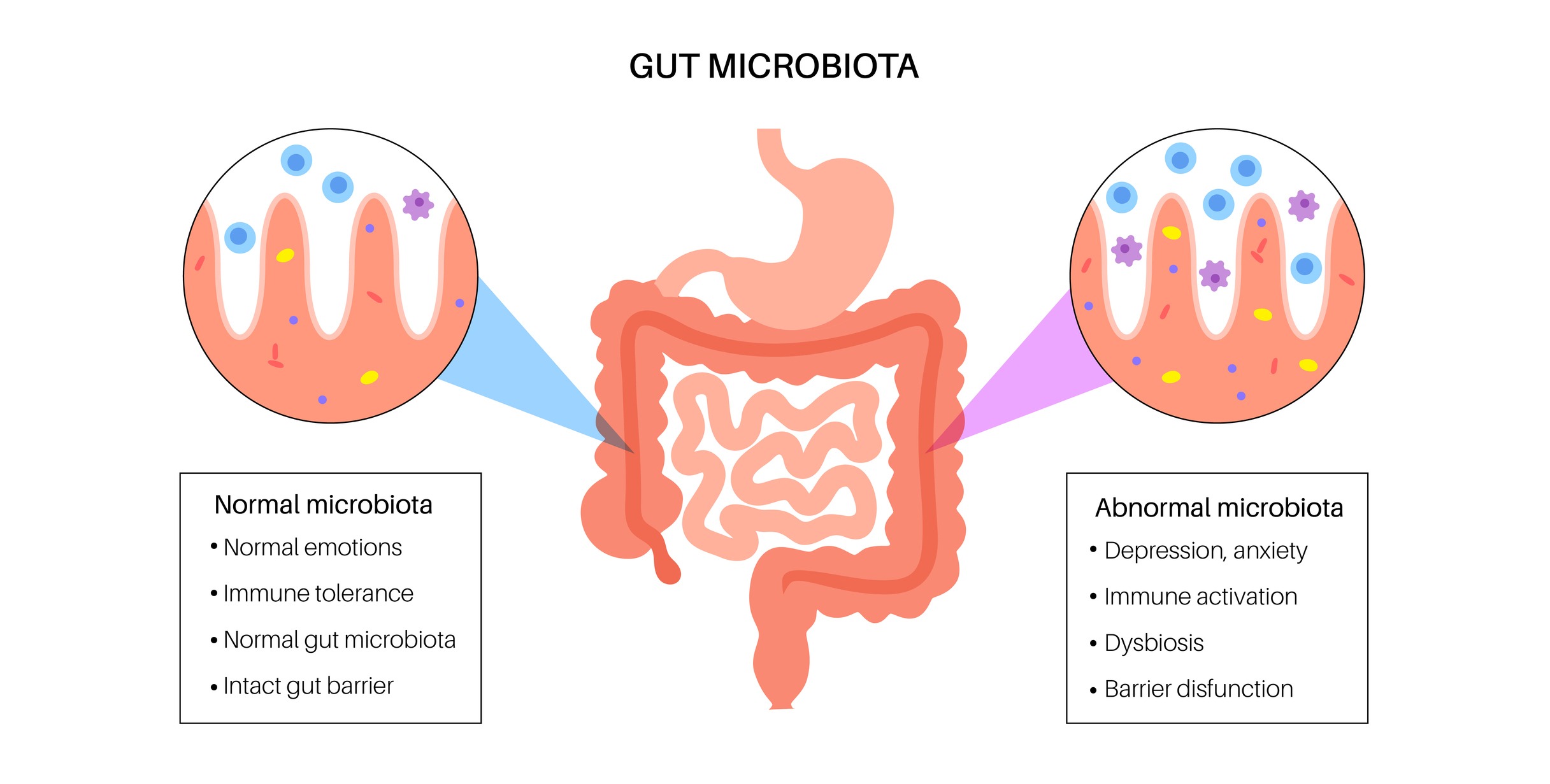
Being an immunocompromised-cancer-survivor, in these days, where COVID is still with us, one of the areas that I think about a lot is immunity. Did you know that about 70% of your immune system, by weight, is in your gut? Your gut is lined with a very fine, single cell, layer of epithelial cells, and below that is gut-associated lymphoid tissues, (GALT). The epithelial cells help support the microbiota, while also helping to keep out invading pathogens. One of the main activities of GALT is to induce an immune response against these pathogens, which includes making antibodies that target these invaders. It is a very fine layer of protection, which can then become compromised, leading to what is known as “leaky-gut-syndrome”. This is where there is damage to the epithelial cells lining the gut, leaving gaps where food and pathogens can enter the blood stream. There is thought that because this dysfunction creates inflammation, and an overreaction of the immune system, it may be responsible for various disorders ranging from IBS, joint pain, mood disorders, various autoimmune diseases and more.
There is much talk lately about the gut-brain connection. The gut-brain axis (GBA) consists of communication between the nervous system and intestinal functions, in both directions. Gut microbiota creates signals to the brain and the brain creates signals back. This complex communication system links emotional and cognitive centers of the brain, with intestinal functions such as immune activation, intestinal permeability and entero-endocrine cell signaling (the production of GI hormones). When this communication system is out of balance, it can have an effect on mood and higher cognitive functions, as well as compromise GI function.
In a healthy person, the helpful, and not so helpful ‘bugs’, can coexist without problems. ‘Dysbiosis’ is the term used, when there is a disturbance in the balance of gut microbiota, which can lead to all kind of problems. Signs of dysbiosis include: heartburn/reflux, diarrhea, constipation, bloating, gas, nausea, food sensitivities, food allergies, fatigue, sinus congestion, skin breakouts, brain fog, as well as ‘leaky-gut-syndrome, mentioned earlier. Prolonged use of antibiotics, or other medications, certain infections, environmental factors, stress, and dietary choices can create dysbiosis. In some people, genetics also has an influence. Each person has their own unique microbiome based on these different factors.
How can you know the state of your microbiome? There are stool tests, generally given by a functional medicine doctor, or other credentialed holistic practitioner, that can give you a huge amount of information on the state of your microbiome. You will know more than you ever imagined about your gut, including the amount and balance of a wide variety of organisms, helpful and not so helpful substances being given off by these organisms, the amount of inflammation being produced, absorption of nutrients, and much more. I’ve had this done twice, several years apart, after being treated for the lymphoma. I could see the impact of the chemotherapy on my gut, and then, after a few years of working to improve things, I retested again, to see where I was. I may do it again this year, as I am having a fair amount of symptoms relating to dysbiosis, that are new to me.
From a dietary perspective, there is a lot you can do to positively influence the health and balance of your microbiome. Anything you consume has an effect on your microbiome, for the better, or for the worse.
A High Fiber Diet affects the type and amount of microbiota in the gut. This fiber is broken down and fermented, by enzymes produced by the microbiota, short chain fatty acids (SCFAs) are then produced, which create a lower pH environment. Certain harmful species of bacteria are less likely to thrive in a lower pH environment. Ideally, the goal is to eat 30 different plant-based foods per week, which is the number that will allow for a diverse and rich microbiome. Different species of microbiota prefer different foods, so, the goal of 30 should satisfy the amount AND diversity of helpful species. If you are just starting out, add new plant-based foods slowly, and in low quantities. If you are not used to eating this way, they may create uncomfortable symptoms such as gas and bloating.
There are Two types of Fiber:
Insoluble Fiber – Also called Prebiotic Fiber, insoluble fiber feeds the beneficial microbiota and, as a result, they support increased levels of SCFAs. Prebiotic fiber is found in a number of foods such as: corn, unripe bananas, beans, cooked potatoes, cooked brown rice that has been cooled down, raw garlic, raw onions, asparagus, apples, kale, celery and wheat bran, and it can also be found in certain supplements.
Soluble Fiber – Dissolves in water to form a gel-like material that adds water and bulk to the stool, to help move things along through the digestive tract. Other benefits include helping to lower inflammation, helping to control blood sugar levels, lower the risk of colon cancer and help you to achieve a healthy weight, by keeping you fuller longer and therefore, more energy dense.
Most Americans do NOT get the recommended amounts of fiber in their daily diets.
The Institute of Medicine recommends the following amount of fiber in your diet per day:
Men Under 50 – 38 grams
Men Over 50 – 30 grams
Women Under 50 – 25 grams
Women Over 50 – 21 grams
NOTE: “… Animal products contain zero amount of fiber. Fiber is ONLY found in plant foods. Humans were meant to eat plants, and lots of them, to keep our gut moving along and happy”.
So then, what are “Probiotics” that we often hear about? These are supplements and foods, that contain live, beneficial microbiota, that can help you maintain a healthy community of microorganisms, in general, or after an illness and/or certain medications. They include fermented foods, such as, yogurt (dairy and plant-based with active live cultures), sauerkraut, tempeh, kimchi, miso, pickled vegetables, kombucha, and cheese (with active cultures). There are numerous probiotic supplements that you can take, and always look for ones with a good variety of organism strains.
So, what “bugs” your microbiome? Antibiotics and other drugs that kill good “microorganisms”. Chemotherapy was needed in my case, but it basically wiped my intestines clean, where I had to start again, developing a healthy microbiome. What also “bugs” your microbiome is a diet high in processed foods and low in fiber, a diet with low diversity of plant foods, GMO foods, foods with added sugar, foods fried in refined vegetable oils (such as canola, soybean and corn), animal protein (especially red meat that raises levels of trimethylamine N-oxide (TMAO), a byproduct of gut bacteria that is linked to a higher risk of developing atherosclerosis).
SUMMARY
The following is a list of the things that can help keep your personal microbiome in check, and thriving:
- Eat a mostly whole-food plant-based diet (90-100% of daily calories).
- Strive for at least 30 different individual plant foods per week. Work up to this slowly, by adding 1 to 2 half-cup servings per week, if you are not used to eating this way. Include cooked and blended foods, to help ease into this way of eating.
- Include fermented foods in your weekly diet.
- Make sure to stay well-hydrated. Check out this calculator here for your personal fluid needs.
- Avoid processed foods, foods cooked in most vegetable oils, GMO foods, and foods with artificial ingredients.
- Avoid toxins of any kind – chemical (i.e., mold, cigarettes, etc.) and emotional (i.e., stress).
- Avoid overuse of medications. Discuss this with your relevant doctor(s).
- Consider adding probiotic supplements to your regimen, as needed. Discuss with your doctor or other health care professional.
- Consider doing a GI stool test, if you suspect dysbiosis or some other dysfunction of your gut. Discuss this with a functional medicine doctor.
- Get regular cancer screenings when appropriate or indicated. Discuss with your relevant doctor(s).
We each have our own personal world of these trillions of organisms that live within us called our ‘microbiome’. If we keep them happy, they keep us happy. Sounds like a fair deal to me!
Below are my sources and some resources to explore this topic further:
How To Cultivate A Healthy Microbiome With Food – Nutritionfacts.org
Human gut-associated lymphoid tissues (GALT); diversity, structure, and function – Nature.com
The Microbiome – Harvard T.H. Chan School of Public Health
Dietary Fiber: Essential for a healthy diet – The Mayo Clinic
Wishing you good health and a great life-
Sheryl
* DISCLAIMER: I am a Certified Health Coach – not a licensed medical professional. The information in this blog post is for informational purposes only and is not meant to diagnose, prevent, treat or cure any disease or condition. It is not intended as a substitute for the advice and treatment and/or diagnosis of a licensed medical professional. Please consult with a licensed medical professional before adopting any new dietary changes.


